Why advance care planning matters

February 21, 2019
By Lisa Brunelle, Communications Advisor, Covenant Health
Do you know what you want to happen if you become really ill? And equally important, do others know what you want?
It’s challenging to make these decisions and then share them with our loved ones as well as our doctor. But it’s important that we do advance care planning, where we think about and share our wishes for future health and personal care.
“The benefit of having a plan is most importantly, I think, that your family has an idea of what it is that you want, so they can guide us, your care team, in how we can accomplish that goal for you,” says Dr. Ella Rokosh, Intensive Care Unit Physician at the Misericordia Community Hospital.
Speak to your doctor or care provider
Make an appointment to sit down with a doctor to ask about your options should you get sick. It’s important to understand your options before you make a decision.
“We have a lot of ways now to keep people alive, but we want to make sure we’re doing what you wish and helping get you to the place you want to be,” says Ella. “We need to understand what quality of life you’d like to preserve because it will help us determine what care we can offer you and when we may need to stop what we’re doing and offer you comfort.”
Make an advance care plan
An advance care plan is a process where you consider what you value in life and in your health and then share your thoughts with family, friends and healthcare providers. If you have an illness, you take time to learn about it. As part of your planning, you appoint a decision maker who will represent your wishes if you’re not able to do so yourself. It is important to document this plan.
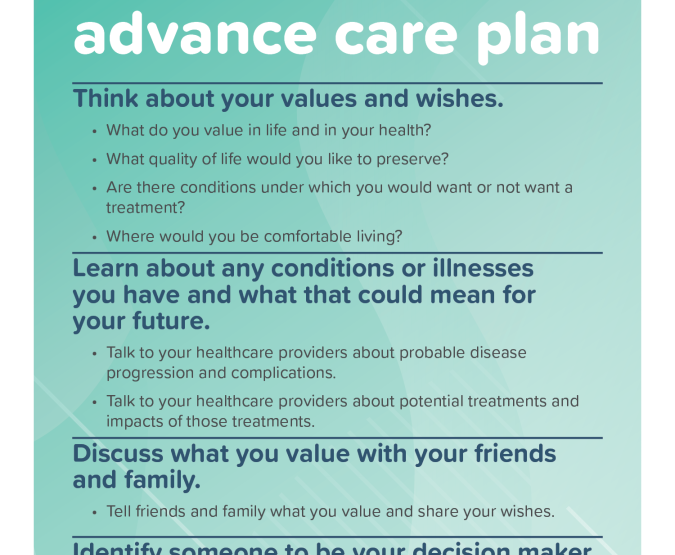
Steps in an advance care plan
Think about your values and wishes
- What do you value in life and in your health?
- What quality of life would you like to preserve?
- Are there conditions under which you would want or not want a treatment?
- Where would you be comfortable living?
Learn about any conditions or illnesses you have and what that could mean for your future
- Talk to your healthcare providers about probable disease progression and complications.
- Talk to your healthcare providers about potential treatments and impacts of those treatments.
Discuss what you value with your friends and family
- Tell friends and family what you value and share your wishes.
Identify someone to be your decision maker if you can't make your own decisions
- Pick someone you trust to represent your wishes and make decisions when it's difficult. This person should be someone who would be comfortable talking to your healthcare team.
- Have a conversation about your wishes with your decision maker.
- Share with your other family and friends who you have asked to be your decision maker.
Document the name of your decision maker and your wishes
- Consider creating a personal directive which is a legal document. A personal directive does not have to have detailed information. The most important part of creating a personal directive is naming your decision maker, your agent. Your healthcare team will support your decision maker regarding the specifics of your health situation.
How the plan helps you and your loved ones
Having an advance care plan in place means loved ones and your doctor know what you want should you fall ill or become unable to communicate your desires. That decision can be a heavy burden if family members don’t understand your wishes.
“If the family has to make decisions for you and they have no idea what your wishes were, they don’t really want to make decisions,” says Ella. “They can be paralyzed by decision-making. Even if they do make decisions, they may feel guilty. That guilt can stay with them beyond the death of their loved one because they don’t feel they accurately spoke for the person and they’ll never know.”
Don’t wait to plan
There’s no need to wait till you’re in your senior years to make an advance care plan. And it’s a plan that can easily be adapted to reflect a change of heart.
“Advance care planning is a conversation, not a one-time discussion,” says Ella. “It’s something that will likely evolve over time as we age, our health changes or our preferences change.”
Be open about your plan
Family members may not want to raise the topic with you. It’s easier if the person with the advance care plan starts the conversation. If someone else is facing a death, illness or injury, that may serve as an opportunity to discuss the topic with loved ones.
“It’s important to share what you want to get out of life with your decision maker and family,” says Ella. “What would you be happy with? For example, if you cannot return home or live independently, would that be OK? It’s more than, ‘I don’t want machines to keep me alive.’”
To learn more about advance care planning, visit Advance Care Planning.
Advance care planning statistics
- Only 20 per cent of Canadians know what an advance care plan is. That means 80 per cent don't know what it is or didn't make one.
- 80 per cent of the time when people are really sick, they can't advocate for themselves.
- 43 per cent of Canadians will have to make decisions while they're dying, but only 30 per cent of them will be able to do so on their own.
- 100 per cent of us will die. Talk with your loved ones to discuss your advance care plan.