Resident care manager shares his COVID-19 experience
August 23, 2021
By Brenton Driedger, Social Media and Storytelling Advisor, Covenant Health
Last November, during the second wave of COVID-19, Javier Martinez drove through a snowstorm from Calgary to Edmonton so he could work at a continuing care site dealing with outbreaks.
Several staff at Chateau Vitaline were in isolation, and Javier, a resident care manager, volunteered to help cover shifts for a few days. But first, he had to go up Highway 2 in his Toyota Corolla.
“I don’t know if I thought too much about what was ahead. It was more ‘Let’s go. Let’s get it done. Let’s help as much as possible.’ First of all, the only thing that was in my head was ‘I need to get through this blizzard.’”
Javier, who works at Covenant Care’s St. Marguerite Manor, was happy to help at the sister facility in Beaumont.
“I did anything that needed to be done,” says Javier, a registered nurse. “I administered medications. I provided bedside care. I provided support with stocking supplies, taking out the garbage, talking to residents and spending time with residents, auditing.”
Like many healthcare workers on the front lines, Javier had both professional and personal encounters with COVID-19. Two days after returning home from Chateau Vitaline, he tested positive for the virus. He believes he was infected by a resident with dementia. He had just left her room after an assessment and was removing his personal protective equipment when she approached him.
“As I removed my mask and my face shield, I looked up, and this resident was just right in my face, talking to me,” says Javier.
“She was just right there in her doorway, smiling at me really close.”
His first swab came back negative, but after he returned home, he developed a fever, headache, cough and body ache, and he got tested again.
Javier describes those initial symptoms as uncomfortable but not overbearing. And while he did his best to keep the virus from spreading, two of his children became infected.
“It’s really difficult when you have five kids. Two of them you have no control of because of their age and their inability to follow directions at their age. I tried to do some semblance of isolation downstairs, but my kids were always coming into my room to play with dad or spend time with dad.”

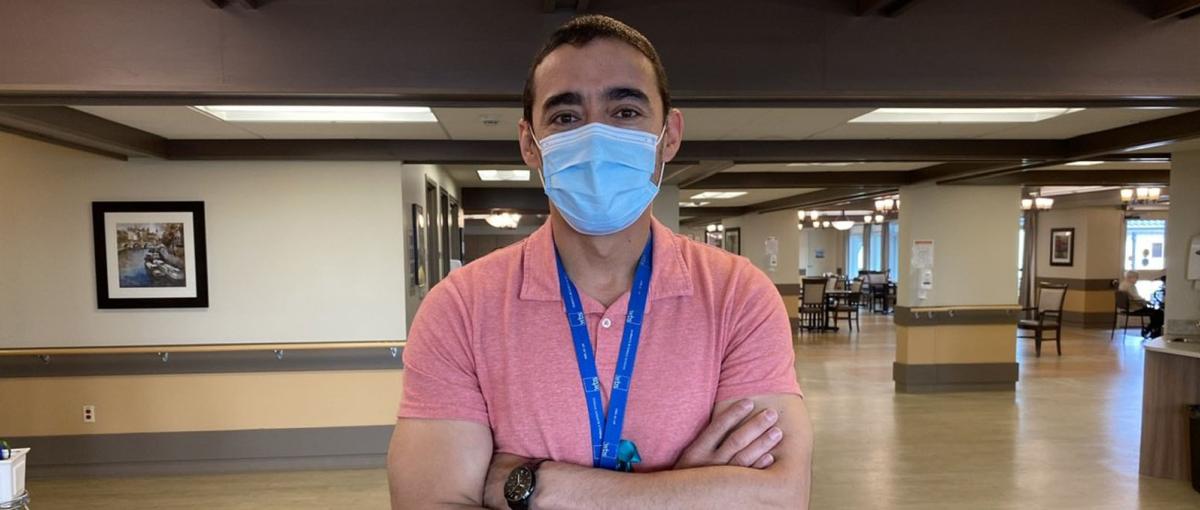
Javier prepares to enter a resident's room.
Javier’s quarantine ended after 10 days, but his family had to isolate for another two weeks. Although spending more time together strengthened the family's bond, Javier developed a deeper appreciation for what residents experience when they isolate alone.
“That was a huge struggle for the family. It was almost a month when you think about it,” says Javier. “We’re fortunate that we’re a large family, and we were able to keep each other entertained, and we had each other. But I cannot fathom people going through COVID alone.”
- Read more: Understanding the toll of COVID-19
Even after Javier’s initial symptoms subsided and his isolation ended, he continued to experience fatigue, mental fogginess and loss of appetite.
“There was this really weird sense of smell, where I constantly had this sense that I could smell BO. I remember I even asked my wife, ‘Do I have a weird body odour?’ And she said, ‘No, you smell fine.’ But that was the constant smell I had. So it’s really difficult to have a decent appetite or to eat when you have this really weird bad body odour constantly with you.”
From his clinical and personal experience, Javier is well aware of both the physical and social effects of COVID-19, and he is grateful for how his Covenant colleagues responded. He says a key factor was bringing in extra staff when residents with dementia tested positive. Those residents tend to wander, which increases the risk of transmission.
“Most of the residents in memory care require more time for redirection,” says Javier. “We brought in extra staff to provide one-to-one care and direction for those residents to make sure they stayed as far away as possible from other residents, keeping them entertained, keeping them in their suites as much as possible. If the staffing wasn’t there, that would have never happened.”
Javier also appreciates how the St. Marguerite team supported his return to work while he was dealing with the after-effects of COVID-19. He says it took a few weeks for him to get back up to speed due to the mental fogginess he experienced.
“I was very fatigued. That was one of my biggest issues. I also noticed that cognitively it was different and that my reaction time was very, very slow,” says Javier. “I gave my team and my boss a heads-up, and they were very supportive of me transitioning in that time.”