Grey Nuns trials new study to treat severe depression
Grey Nuns trials new study to treat severe depression

November 23, 2020
By Karen Cho, Senior Communications Advisor, Covenant Health
A first of its kind clinical trial to study a new treatment for severe depression is being piloted at the Grey Nuns Community Hospital.
Dr. Michael Demas, who is spearheading the study with lead researcher Dr. Raheem Suleman, says the trial is especially important given the mental health impacts of the COVID-19 pandemic. Recruitment for the trial was halted in April but recently restarted with all the safety and hygiene precautions in place.
“The pandemic has emphasized that this condition exists in our population,” says Michael, a psychiatrist at Grey Nuns Community Hospital and associate clinical professor at the University of Alberta.
He believes anecdotal evidence also points to increasing challenges people are facing as a result of the pandemic. Poor mental health can lead to depression. Even before COVID-19, depression affected approximately 11 per cent of men and 16 per cent of women in Canada.
While there are many treatments, including medication and talk therapy, about one in five Canadians continue to be resistant to them. Raheem believes the pandemic has increased awareness — and acceptance — of depression.
“The COVID pandemic has had an immense impact on society and has brought a renewed focus on mental health, which may help to destigmatize depression.”
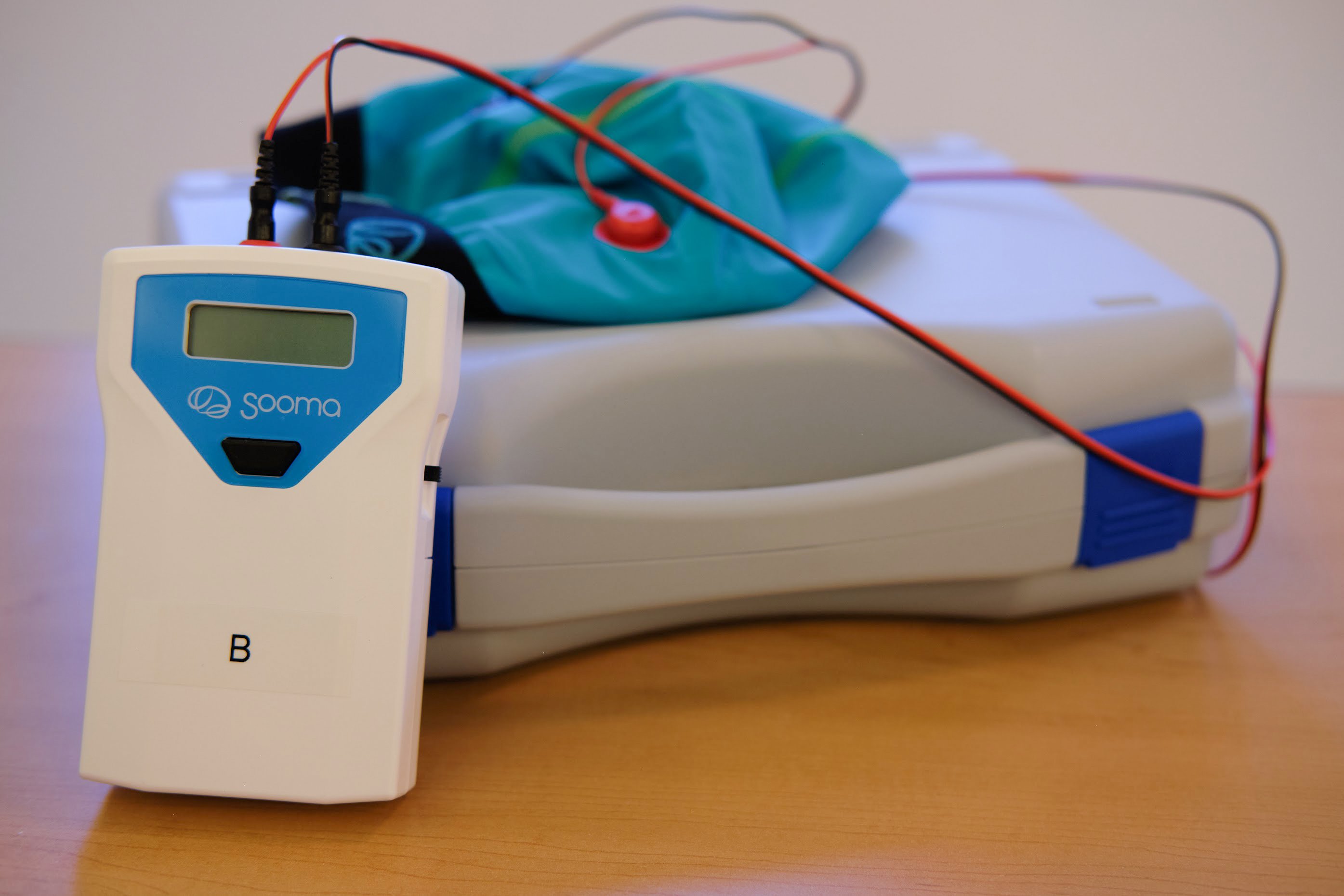
The clinical trial is investigating whether a non-invasive method of electrical stimulation, known as transcranial direct current stimulation (tDCS), can be effectively used to treat this level of ultra-resistant depression. Both Michael and Raheem say this method is different from the traditional electroconvulsive therapy (ECT), which uses electricity to generate a medically supervised seizure but has had documented side effects for some patients.
With tDCS, electrodes are applied directly to the scalp, and a low-intensity electrical current is delivered for up to 30 minutes. Unlike ECT, this treatment doesn’t require patients to be anaesthetized or put under or to stay in hospital.
Using the analogy of the brain as a chemical electrical machine, Michael explains that in depressed persons parts of the brain are slowed down or even shrunk, so the number of connections in these areas are reduced. tDCS is a direct way of getting into the brain with electricity, functioning like a cheerleader to encourage depressed areas to speed up or slow down.
Participants in the clinical trial will be randomly assigned to two different groups. Those in the intervention group will receive 30 sessions of active tDCS and 30 minutes of electrical stimulation per session, while those in the control group will receive 30 sessions of sham tDCS. The electrodes will be applied for 30 minutes to all participants to mimic conditions in the placebo group.
This is also a double-blind study, where neither participants nor investigators will know which group participants belong to. Participants will also continue to take previously prescribed medications.
Michael says extra precautions will be taken during the trial to mitigate the risk of COVID-19. For example, all participants will be screened at the main entrance of the Grey Nuns Community Hospital and again before entering the treatment area, and all equipment will be thoroughly sanitized between applications.
“What drives me is the people I see who are suffering and their families and the desire to find something better for them.”
Raheem adds that the size and scope of the clinical trial are what make it groundbreaking. “The studies that have been done have been kind of underpowered. They didn't look at enough people. They didn’t treat it for a long enough period of time to really say whether or not the treatment works. This is the biggest study for treatment-resistant depression and also the first of its kind looking at ultra-resistant depression.”
There is also a linguistic component to this trial that is also unprecedented. Participants will engage in interviews with the researchers during their sessions, and the data from the interviews will be analyzed differently. “When you are depressed, you change the way you speak. Your processing speed goes down, and your pitch is higher,” explains Raheem.
Michael says ultra-resistant depression takes a heavy toll on families. For example, a teenager may have to skip high school to care for a parent, or a spouse may miss work because of a depressed partner. That can also mean a drop in income levels.
“The tendrils of depression are reaching very deep into society, and it’s becoming one of the most challenging conditions that we have, so we do want to have better treatments,” he says. “This study puts us one more step in the right direction.”