Embracing palliative care
Life circumstances transform caregiver into a palliative care advocate

May 11, 2023
By Ben Freeland, Communications Advisor, Covenant Health
Bill Zheng was only 17 years old and in high school when he suddenly found himself in the position of being his mother’s primary caregiver and healthcare advocate. She had been diagnosed with decompensated cirrhosis (severe scarring of the liver) resulting from Hepatitis B. With his father working long hours to support the family, his grandparents unable to speak English and no siblings to lighten the load, it fell to Bill to help his mother ― who suffered from schizophrenia and also spoke limited English ― navigate the health system.
After his mother had spent half a year in hospital with no sign of improvement, Bill began investigating alternatives to the aggressive treatment she was receiving. When he heard in passing about palliative care, he took it upon himself to learn more and to eventually set up palliative homecare for his mother. His first meeting with the palliative care physician was a breath of fresh air, he says.
“All of a sudden, the conversation was about quality of life, about ensuring that the things most important to [my mother] were prioritized while care continued."
"In my mother’s case, I knew that what she valued most was being at home and eating the kinds of food she liked, and I was able to advocate for that. While at the very end she had to be admitted to hospice, most of this time was at home. I’m happy that she got the kind of care I knew she wanted.”
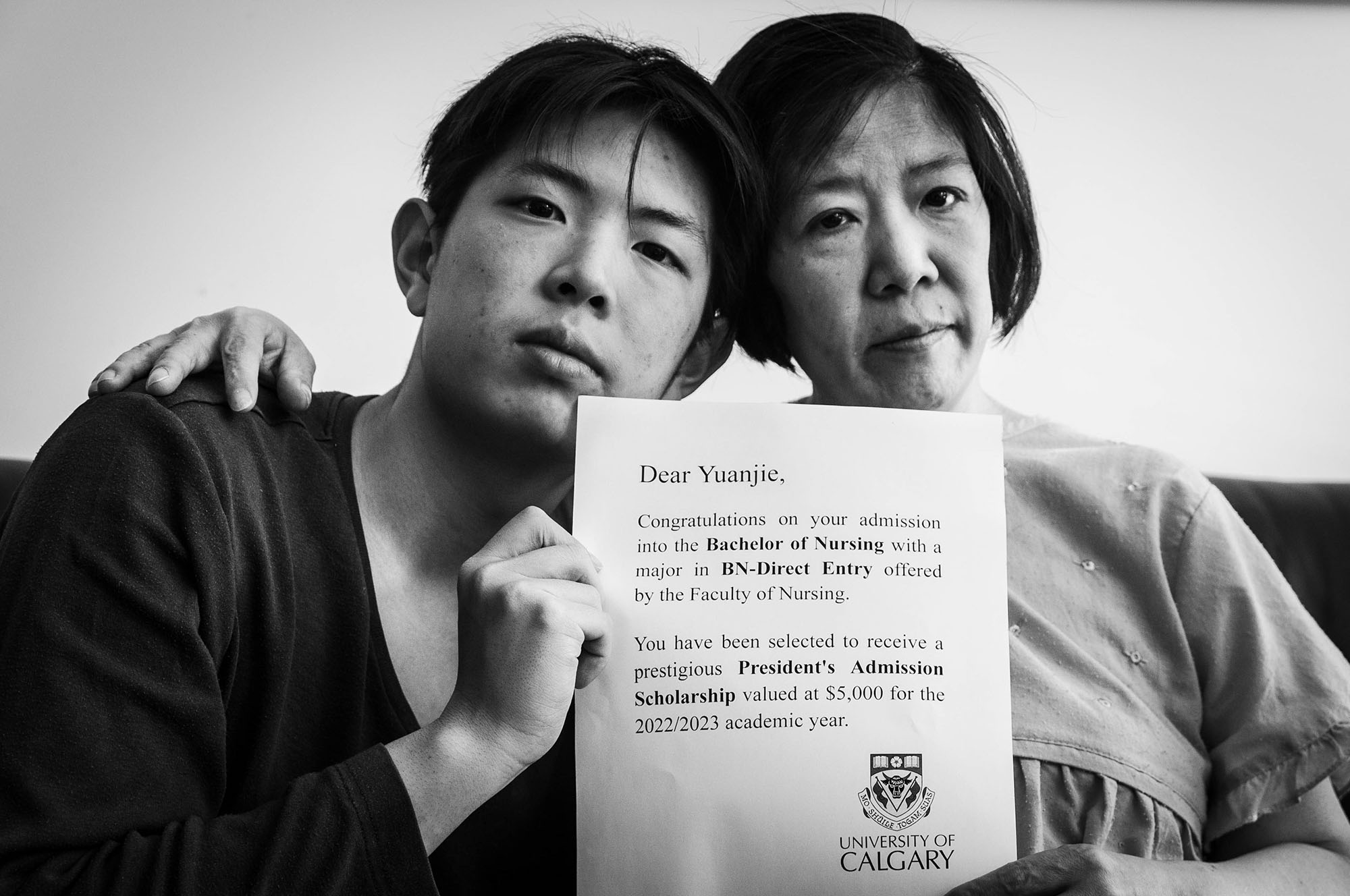
Bill’s mother died in May of 2022, a year and a half following her diagnosis. The journey of being her caregiver led Bill to become an advocate for palliative care. Now 19 and a nursing student at the University of Calgary, he volunteers with the public panel for the Covenant Health Palliative Institute’s Palliative Care Public Awareness project. He contributed his personal story to an online module called Understanding Palliative Care launched on the project’s Compassionate Alberta website this month.
Bill’s story is one of incredible resolve and determination to do the right thing, as well as of the steep learning curve so many people face when dealing with a serious illness for the first time. He shared it in the Understanding Palliative Care module to spread the message that palliative care is beneficial to anyone with a chronic condition and should be made available to anyone who might benefit from it.
“Palliative care is a wraparound service that covers social services together with medical treatment,” he explains. “It really takes into consideration a person’s social situation ― their family structure, personal contacts, financial situation and so on. When we first entered palliative care, I had no idea what to expect, but the first question the palliative physician asked was, ‘What do you want to see at this very critical time, through end-of-life care?’ And from that point on, we felt very supported ― from pain management to developing a consistent schedule for hospital visits to transportation ― on every level.”
Bill also asserts that accessing palliative care shouldn’t be viewed as giving up, noting that this view is particularly prevalent in his own Chinese culture, in which taboos around addressing end-of-life issues often result in patients continuing to undergo aggressive treatments when they have exceeded their medical usefulness.
“Palliative care is not a death sentence. It’s patient-focused and patient-centred care that really values not just western medical interventions but also the values of the patient and their family and loved ones. It’s not giving up. It gives you a better chance of living not only better but longer. And the earlier it’s accessed, the better. In my mother’s case, if I’d known more about palliative care beforehand, I would have pushed for it sooner, but I’m thankful she got the care she deserved.”
Bill may have been thrust into a role that few teenagers find themselves in, but thankfully he didn’t have to walk this road alone. He is grateful to the medical professionals and many others who helped him navigate this difficult time in his life.
“I had a lot of support,” he says. “First of all, there was the hepatologist who introduced me to the idea of palliative care. There was the palliative care physician who talked me through the options. The palliative homecare nurse was the most loving, caring person you could hope for and was very much on top of everything in terms of referrals and forwarding information my way. Thanks to her, we were able to do so much at home. I also had a grief counsellor, who helped me deal with the bereavement process.”
He also notes that he received tremendous support from family friends and others within his own network.
“Transportation was a challenge because I didn’t drive at the time, my father was unavailable and my grandparents couldn’t drive, but thankfully I was able to get rides to and from the hospital from family friends. I was also able to crash at a family friend’s house from time to time when I needed an escape from home. Also, all my teachers knew what was going on and were very supportive. I was excused from exams because of my mother’s death.”
This support, plus the knowledge that he had been a strong advocate for his mother, made the grieving process a lot easier than it otherwise would have been, he says.
“Thanks to my grief counsellor, and my own research, I understood anticipatory grief, and by the end, I had pretty much processed everything. The grieving process was made easier by the fact that I had been such a strong advocate ― both for my mother and for myself.”
About Understanding Palliative Care
Understanding Palliative Care is a multimedia learning module developed by the Palliative Institute to improve public understanding of palliative care in Alberta. Inspired by a public educational module created by the All-Ireland Institute of Hospice and Palliative Care, it features clips from interviews with three people who have personally benefited from palliative care.
Understanding Palliative Care was developed in consultation with palliative care specialists from nursing, medicine and social work, with feedback from the public panel incorporated. The module highlights four areas of support ― physical, emotional, social and spiritual ― that palliative care offers as well as the benefits of early palliative care, which can be received along with other treatments to cure or control a disease. Its messaging is overwhelmingly positive, with the goal of encouraging people to appreciate the benefits of this oftentimes poorly understood area of health care.
To access Understanding Palliative Care, visit the Compassionate Alberta website.